

Pulse Oximeters
Why You Might Want One at Home
A Simple Device That Could Save Your Breath
Monitoring your oxygen levels might not seem necessary—until you can’t catch your breath. Whether you're managing asthma, recovering from COVID-19, or supporting someone with chronic obstructive pulmonary disease (COPD), knowing your blood oxygen saturation (SpO₂) in real-time can be a game-changer. Pulse oximeters, once reserved for hospital settings, are now affordable, accurate, and compact enough to keep in your medicine cabinet.
With respiratory illness on the rise and more people managing chronic conditions at home, pulse oximeters offer a non-invasive window into your respiratory health. This guide will explain how they work, who should consider owning one, how to use them correctly, and what the numbers actually mean—so you can act quickly if your oxygen drops too low.
What Is a Pulse Oximeter and How Does It Work?
A pulse oximeter is a compact, battery-powered medical device designed to measure two vital indicators of respiratory and cardiovascular health: your blood oxygen saturation (SpO₂) and pulse rate. The device typically clips onto your fingertip, though models for earlobes, toes, and even wrist-worn versions exist. Because it’s non-invasive, painless, and offers fast results, pulse oximeters are now commonly found in homes—not just hospitals.
What SpO₂ Means
SpO₂ stands for peripheral capillary oxygen saturation—an estimate of the amount of oxygenated hemoglobin in your blood. Hemoglobin is the protein in red blood cells that binds to oxygen. The percentage shown on a pulse oximeter reflects how much of your hemoglobin is saturated with oxygen.
A normal SpO₂ reading typically ranges from 95% to 100%.
Readings between 90% and 94% may be acceptable for people with chronic lung conditions but should be monitored closely.
Readings below 90% are considered low (hypoxemia) and usually warrant immediate medical attention.
Why does this matter? Oxygen is essential for every cell in your body. When oxygen saturation drops, organs—including your brain and heart—can be deprived of the oxygen they need to function, especially during respiratory illnesses or flare-ups.
How It Measures Oxygen
Pulse oximeters use photoplethysmography, a light-based technology, to assess how oxygen-rich your blood is. Here’s how it works:
Red and infrared light pass through the tissue (usually a fingertip).
Sensors on the other side measure how much light is absorbed.
Oxygenated and deoxygenated hemoglobin absorb light differently:
Oxygenated hemoglobin absorbs more infrared light and allows more red light to pass through.
Deoxygenated hemoglobin absorbs more red light and allows more infrared light to pass through.
The device uses these light absorption differences to calculate your SpO₂ and your pulse rate, displaying both values within seconds.
Additional Features on Modern Devices
Pleth waveform: A graph that shows pulse strength over time.
Perfusion index (PI): Indicates how well blood is flowing through the measured area.
Bluetooth syncing: For storing data via smartphone apps.
In short, this simple device uses advanced optical science to give you crucial health insights—instantly and painlessly.
Who Should Consider a Pulse Oximeter at Home?
Pulse oximeters were once standard only in hospital ICUs and emergency rooms. Today, they’re commonly found in homes across the globe, particularly after the COVID-19 pandemic highlighted their usefulness for tracking respiratory health.
Here are the groups that may benefit most from owning a pulse oximeter at home:
1. People With Asthma
Asthma causes narrowing of the airways, which restricts airflow and can lead to a drop in oxygen levels—especially during an attack or severe flare-up. For individuals with moderate to severe asthma:
A pulse oximeter can provide a clear, objective indicator of whether their oxygen is dropping, even before symptoms worsen.
It allows for timely use of rescue inhalers or corticosteroids.
Helps monitor response to treatment at home, potentially avoiding unnecessary ER visits.
2. People With COPD or Other Chronic Lung Conditions
Chronic Obstructive Pulmonary Disease (COPD), emphysema, and chronic bronchitis can impair gas exchange in the lungs, leading to chronically low oxygen levels. For these individuals:
A pulse oximeter helps track daily baseline SpO₂ and notice deviations early.
It supports oxygen therapy titration (for those on supplemental oxygen).
Can be used during pulmonary rehabilitation or light home exercise to ensure safe oxygenation.
Regular monitoring helps avoid exacerbations and improves long-term outcomes.
3. COVID-19 or Long COVID Patients
One of the most troubling features of COVID-19 is silent hypoxia—a condition where blood oxygen levels fall dangerously low without obvious symptoms. People feel “fine” until their condition suddenly deteriorates.
For COVID patients recovering at home:
Pulse oximeters allow early detection of oxygen decline—even before shortness of breath starts.
Patients and caregivers can decide when to escalate to medical care based on real-time data, not guesswork.
For Long COVID sufferers, oximeters can track post-exertional oxygen drops, helping to avoid overexertion and flare-ups.
4. Post-Surgery or Illness Recovery
After procedures involving anesthesia or hospitalizations for pneumonia or flu, oxygen levels may remain unstable for days or weeks. Monitoring SpO₂ at home during recovery:
Helps ensure that respiratory function is returning to normal.
Alerts you early if complications are developing, such as a pulmonary embolism or infection relapse.
Can provide reassurance for patients recovering from cardiac or thoracic surgeries.
5. Athletes and High-Altitude Travelers
Some endurance athletes—especially cyclists, runners, and triathletes—use pulse oximeters to:
Monitor how their body is responding to strenuous workouts or hypoxic training.
Avoid dangerous oxygen dips during intense training sessions or competitions.
Ensure adequate oxygenation during altitude training or climbs above 7,000 feet.
For hikers, climbers, or skiers spending time at high elevations, oximeters are useful to detect early signs of altitude sickness or acute mountain sickness (AMS).
How Fitness and Endurance Athletes Can Benefit from Pulse Oximeters
While pulse oximeters are most commonly associated with clinical care, they also have practical value for athletes—especially those training at high intensity, performing endurance sports, or exercising in challenging environments like high altitudes. Used correctly, they can help you optimize training intensity, monitor recovery, and prevent overexertion.
Why Oxygen Saturation Matters in Training
During exercise, your body demands more oxygen. Efficient oxygen delivery is crucial for performance, especially in aerobic sports like:
Running
Cycling
Rowing
Triathlon
CrossFit
Hiking or climbing at altitude
By tracking your SpO₂ before, during, or after workouts, you can:
Gauge how well your body is oxygenating under stress
Spot early signs of fatigue or overtraining
Monitor recovery status and readiness to train again
How to Use a Pulse Oximeter in Training Contexts
✅ Pre-Workout Baseline Checks
Measure your SpO₂ and pulse at rest before training. If your oxygen level is unusually low (below your typical range), it could indicate:
Incomplete recovery
Poor sleep
Illness
Altitude effects
Training under these conditions may increase the risk of poor performance or injury.
✅ Post-Workout Recovery Monitoring
After intense cardio sessions or high-volume strength training, your oxygen saturation may temporarily dip due to elevated heart rate or respiratory stress. Monitoring post-exercise SpO₂:
Helps evaluate how quickly you return to baseline
Can identify if you're under-recovered or pushing too hard
Supports data-driven recovery protocols (e.g., active recovery vs. rest day)
✅ Altitude Training and Acclimatization
For athletes training above 5,000 feet (1,500 meters), pulse oximeters are essential for:
Tracking adaptation to altitude
Avoiding altitude sickness
Balancing training load with recovery
A drop in SpO₂ at altitude is normal, but if it dips below 88–90%, performance suffers and health risks increase.
Tips for Trainers and Coaches
Track trends, not just single readings. Is an athlete’s SpO₂ dropping more than usual after intervals? Are they recovering slower this week?
Correlate readings with RPE (Rate of Perceived Exertion) to validate subjective vs. objective fatigue.
Use SpO₂ monitoring alongside HRV (heart rate variability) or resting heart rate to build a comprehensive recovery dashboard.
For group training environments, pulse oximeters can help identify at-risk clients who may be pushing beyond their safe limits—especially in heat or altitude.
When Not to Use It
Pulse oximeters aren't ideal during vigorous movement, such as during the actual workout, because motion artifacts can distort readings. Always test at rest or in recovery.
Conclusion for Athletes
A pulse oximeter may not directly make you faster or stronger—but it offers a clearer picture of your physiological status, so you can train smarter, recover faster, and reduce the risk of burnout. For elite athletes or weekend warriors, it’s a small investment with big returns.
SpO₂ vs. VO₂ Max — Oxygen Monitoring vs. Oxygen Performance
If you’re active in endurance sports or serious about optimizing your training, you’ve probably come across both SpO₂and VO₂ max. While they both relate to oxygen, they serve very different purposes—and understanding how they work can help you use each tool more effectively.
What’s the Difference?
🩸 SpO₂ (Peripheral Capillary Oxygen Saturation)
SpO₂ refers to the percentage of hemoglobin in your blood currently carrying oxygen. It’s a real-time snapshot of how well your lungs are delivering oxygen into your bloodstream—especially relevant during illness, recovery, altitude changes, or respiratory stress.
Measured by: Pulse oximeter (fingertip clip)
Normal range: 95–100% at rest
Use cases: Medical monitoring (asthma, COPD, COVID), altitude adaptation, post-workout recovery
🫁 VO₂ Max (Maximal Oxygen Uptake)
VO₂ max is a measure of how much oxygen your body can actually use during peak exercise. It’s considered one of the best indicators of cardiovascular fitness and endurance capacity, and is often used to track athletic performance over time.
Measured by: Lab testing with mask and treadmill, or estimated via fitness trackers
Typical range:
Untrained: 30–40 ml/kg/min
Trained endurance athletes: 60–85+ ml/kg/min
Use cases: Endurance training, performance testing, training progress tracking
Think of It Like This:
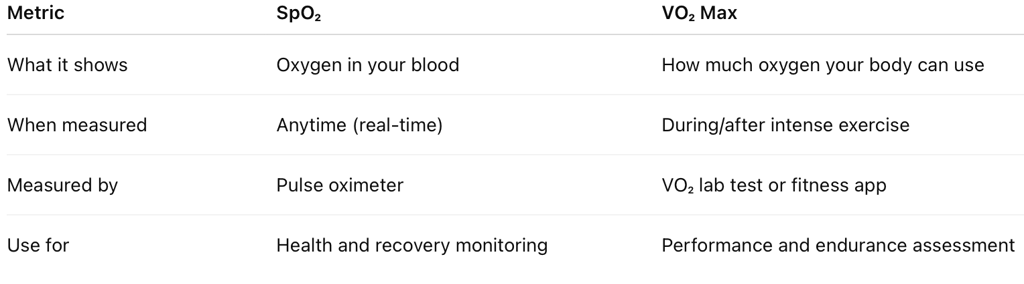

Complementary, Not Interchangeable
SpO₂ = Oxygen availability
VO₂ max = Oxygen utilization
In other words, SpO₂ tells you how much oxygen is getting into your blood, while VO₂ max tells you how efficiently your body can use that oxygen during physical exertion.
For athletes and trainers, both metrics have value:
Track SpO₂ to ensure you’re training and recovering safely, especially in high-altitude, heat, or illness-recovery scenarios.
Train to improve VO₂ max to enhance aerobic endurance and overall performance.
What Is a Normal SpO₂ Reading?
Your SpO₂ level reflects how well oxygen is being delivered throughout your body, and it's one of the fastest ways to assess respiratory efficiency. In most healthy individuals, a normal resting SpO₂ reading should fall between 95% and 100%. This indicates that the majority of hemoglobin in your red blood cells is carrying oxygen effectively.
Understanding the Numbers:
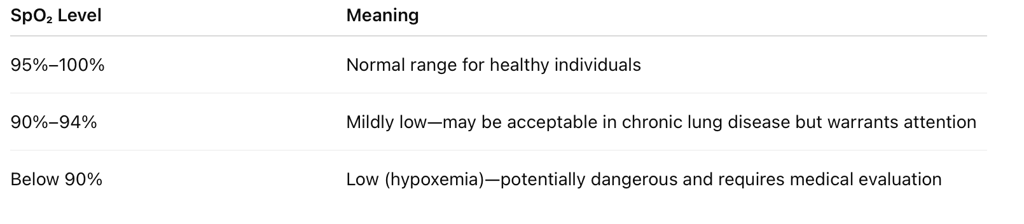
It’s important to remember that some people with chronic respiratory conditions, such as COPD, may live with slightly lower baseline readings. However, any sudden drop or consistently low value—especially below 90%—should prompt you to seek medical advice.
Also note that factors like cold hands, nail polish, or poor circulation can affect accuracy. Always interpret your SpO₂ reading in context—paired with how you feel, your known health conditions, and current symptoms.
How to Use a Pulse Oximeter Correctly
While pulse oximeters are incredibly easy to use, accuracy depends on a few important steps. Environmental conditions, improper finger placement, or even nail polish can throw off the reading. To ensure you’re getting a reliable result, follow this step-by-step guide.
Step-by-Step Instructions:
Rest Before Measuring
Sit quietly for at least 2–5 minutes before taking your reading. Physical activity, stress, or even talking can temporarily raise your heart rate and affect the reading.Choose the Right Finger
The index or middle finger of your non-dominant hand typically works best. Avoid using fingers that feel cold or have poor circulation.Place on a Clean, Bare Finger
Remove nail polish, artificial nails, or gloves before use. These can interfere with light transmission and lead to falsely low readings.Ensure Proper Placement
Insert your finger fully into the oximeter, making sure the sensor covers the fingertip pad. The device should not feel too loose or tight.Stay Still and Quiet
Hold your hand steady and avoid movement, talking, or clenching your muscles. Motion can disrupt the photoplethysmography process and distort results.Wait for a Stable Reading
Allow the numbers to stabilize—this may take 5 to 15 seconds. Many devices show a pulse bar or waveform to indicate measurement quality.Record Both SpO₂ and Pulse Rate
Note the SpO₂ (%) and pulse (BPM) readings. If you’re monitoring over time, write it down with the date, time, and any symptoms.
Avoid These Common Mistakes:
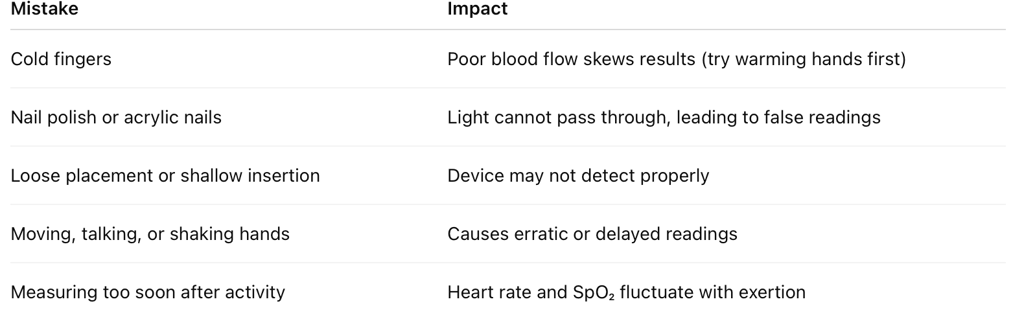
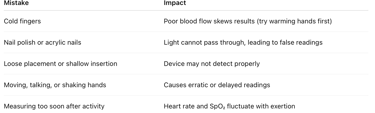
Tip: For consistent tracking, measure at the same time each day under similar conditions.
What If My Oxygen Saturation Drops?
Seeing a lower-than-normal SpO₂ reading can be alarming, but context is key. A single reading below 94% doesn’t always indicate a crisis—unless it’s accompanied by symptoms. However, consistent or sharp drops in oxygen saturation should never be ignored, especially if you have underlying respiratory or cardiac conditions.
When to Monitor Closely:
If your reading falls below 94%:
Recheck the reading after a few minutes of rest.
Ensure your finger is warm and still.
Consider whether you're experiencing any new or worsening symptoms.
If your SpO₂ remains below 94%, or if it drops below 90%, seek medical attention. This level of oxygen saturation is classified as hypoxemia, and may require supplemental oxygen or urgent evaluation.
Emergency Signs That Warrant Immediate Medical Attention:
SpO₂ under 90%, especially with shortness of breath
Rapid or irregular heartbeat
Chest pain or tightness
Blue or grayish lips, fingertips, or face
Confusion, dizziness, or fainting
Breathing difficulty even while resting or lying down
These symptoms suggest that your body isn’t getting enough oxygen to function safely. Don’t wait—call your doctor or emergency services if you’re concerned.
When in Doubt, Trust Your Symptoms
Some people obsess over numbers, but your physical symptoms matter most. If you feel unwell, especially if you're high-risk (asthma, COPD, post-COVID), it's better to act early than delay care.
Choosing a Reliable Pulse Oximeter
With so many pulse oximeters available online and in stores, choosing the right one can be overwhelming. Here’s how to ensure you get a device that’s accurate, durable, and easy to use.
Key Features to Look For:
✅ FDA Clearance or CE Certification
This ensures the device meets medical-grade standards for safety and accuracy.✅ Accuracy Within ±2%
A good oximeter should have an accuracy range of ±2% compared to clinical devices. For example, if your true SpO₂ is 95%, a reading between 93% and 97% is acceptable.✅ Clear LED or OLED Display
Look for large, bright displays that are easy to read—even in low light or for older adults.✅ Battery Life and Power Options
Choose between replaceable (AAA) or rechargeable batteries. Rechargeable models with USB ports are more eco-friendly.✅ Speed and Readout Stability
Avoid models that take longer than 10–15 seconds to stabilize or give erratic results under steady conditions.✅ Optional Extras (if needed):
Bluetooth or app syncing
Data storage for trend tracking
Plethysmographic waveform (shows signal strength)
Perfusion index display
Popular and Trusted Models:
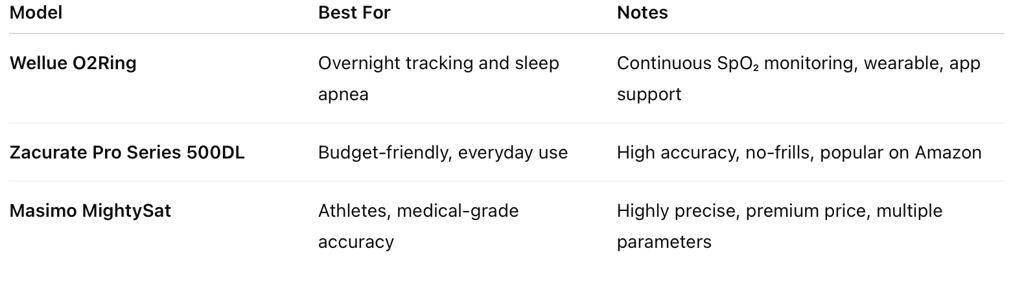
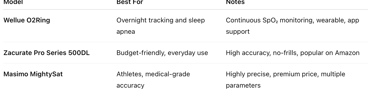
Tip: Always buy from reputable retailers or directly from the manufacturer to avoid counterfeit devices.
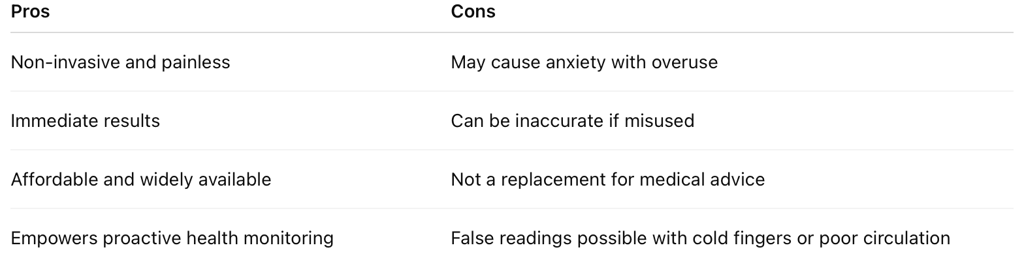
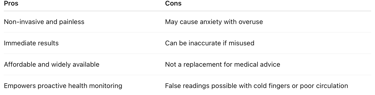
Pros and Cons of At-Home Pulse Oximeters
When to Talk to Your Doctor
While pulse oximeters are incredibly useful for at-home monitoring, they are not a substitute for clinical judgment. The device gives you a snapshot of your blood oxygen level, but interpreting what that means—especially in the context of chronic illness or new symptoms—requires professional insight.
If your SpO₂ consistently reads below 94%, or if you experience other concerning signs, it's important to seek medical advice. Don’t rely solely on the numbers—how you feel matters just as much.
You should consult a healthcare provider if:
You have asthma or COPD and notice increased shortness of breath, chest tightness, or a drop in your usual SpO₂ range.
You're recovering from COVID-19, the flu, or another respiratory illness and experience persistent fatigue, difficulty breathing, or oxygen saturation that dips below 94%.
You have cardiovascular conditions (like heart failure or arrhythmia) and start experiencing irregular pulse readings or reduced SpO₂.
You’re on supplemental oxygen and feel your therapy isn’t controlling symptoms adequately.
You notice symptoms such as lightheadedness, confusion, or chest pain, even if your oxygen readings appear normal—this could point to underlying circulation or neurological issues that the oximeter won't detect.
Even if you feel okay, it’s worth discussing your readings with your doctor during regular checkups—especially if you're using a pulse oximeter as part of a chronic condition management plan. They can help you set baseline expectations, determine your action thresholds, and adjust medications or oxygen therapy as needed.
Can Pulse Oximeters Help Save Lives?
Absolutely. One of the most important lessons from the COVID-19 pandemic was the lifesaving value of early detection—especially for a condition like silent hypoxia, where people’s oxygen levels fell dangerously low before they noticed any symptoms.
Pulse oximeters provided:
Early warnings that prompted timely hospital visits before respiratory failure.
A sense of control for patients managing illness at home, reducing panic and uncertainty.
An essential screening tool for caregivers, telemedicine providers, and those monitoring loved ones from a distance.
In rural areas or overwhelmed healthcare systems, pulse oximeters became a lifeline—helping triage care, allocate resources, and determine who needed emergency intervention.
However, they work best as part of a broader home health toolkit, which might include:
A digital thermometer (for tracking fever)
A blood pressure monitor (especially for heart patients)
A medication tracker or symptom diary
Clear instructions from your healthcare provider on when to act
Pulse oximeters are not just devices—they’re part of a proactive health strategy that empowers patients to take earlier, smarter action.
Final Tips for Everyday Use
To get the most out of your pulse oximeter and avoid false alarms, follow these smart usage tips:
Measure with Purpose
Don’t obsessively check your oxygen throughout the day. Instead, take readings when you:
Feel short of breath
Are recovering from illness
Are monitoring a diagnosed condition
Are adjusting medications or oxygen flow
Keep a Monitoring Log
Use a notebook or app to record:
Date and time
SpO₂ and pulse rate
Symptoms or activity at the time
This log helps you and your doctor see trends over time—far more useful than isolated readings.
Know When to Share Data
Contact your doctor if:
Your SpO₂ dips below your normal range consistently.
You see fluctuations without explanation.
You experience symptoms like dizziness, confusion, or palpitations, even with a “normal” reading.
Also, make sure your loved ones know how to use the device correctly, especially if you’re high-risk or recovering at home.
