
Training Hard with Heart Failure
A Guide for Lifelong Athletes
Embracing a New Chapter in Your Athletic Journey
For those who’ve lived in the gym, on the track, or under a loaded barbell, your identity is built on performance, progress, and power. You’ve trained through injury, setbacks, plateaus — always pushing forward. But now, the challenge in front of you isn’t just physical. It’s internal. It’s cellular. It’s in your heart.
A diagnosis of Heart Failure with Reduced Ejection Fraction (HFrEF) hits differently when you’ve been active your whole life. It’s not just a medical condition — it’s a direct threat to the one thing that’s always kept you grounded: your ability to move, train, and thrive through fitness.
“Can I still train?”
“Will I lose all the strength I’ve built?”
“How hard is too hard now?”
“What does progress even look like from here?”
These are the questions no one hands you answers to. Most advice is written for sedentary people trying to get back on their feet — not for athletes who’ve lived and breathed performance. The default approach of “just walk more” or “try some light stretching” simply doesn’t cut it when you’ve spent your life under a bar or chasing PRs.
But here’s the truth: you can still train — with intensity, purpose, and progress. It will look different, but it will still challenge you. You just need a new playbook — one that respects your diagnosis, adapts your strategy, and keeps your body moving with intelligence and intention.
In this guide, we’ll show you how to:
Restructure your training without giving up the athlete mindset
Scale intensity, rep ranges, and volume to match your cardiovascular reality
Identify which lifts, splits, and intensities to modify, keep, or drop
Find new metrics of progress that fuel your drive
And most importantly — redefine what it means to train hard, without training recklessly
You may be facing limits you never asked for — but those limits don’t erase who you are. This is still your body. Your strength. Your fight. Let’s channel it.
Understanding Heart Failure in the Athletic Context
Heart failure is often misunderstood — especially in athletic circles. It doesn’t mean your heart has stopped working; it means your heart isn’t pumping blood as efficiently as it should. Specifically, in Heart Failure with Reduced Ejection Fraction (HFrEF), the heart’s left ventricle loses its strength, reducing the amount of blood ejected with each beat. In clinical terms, an ejection fraction below 40% typically indicates HFrEF.
To the average person, this translates into fatigue, shortness of breath, reduced exercise tolerance, and swelling in the legs or abdomen. But for lifelong athletes, it’s more than just a physical limitation — it’s a mental and emotional disruption. You’re used to pushing through barriers. Now, your barrier is your own heart.
Why HFrEF Hits Athletes Differently
You’re already conditioned. Standard cardiac rehab protocols — designed to get sedentary individuals moving — can feel insultingly basic.
You’re used to intensity. Dialing it down doesn’t come naturally, and the fear of “losing progress” can lead to denial or risky behaviors.
You know how to suffer. Which means you’re more likely to ignore early signs of cardiac strain or overtraining.
You track performance. So it’s frustrating when your metrics tank or fluctuate for reasons outside your control.
But here’s the good news: athletes often adapt better than non-athletes after a diagnosis — when they have the right tools and mindset. Your body is resilient, your baseline fitness gives you an edge, and your training discipline can help you stay consistent through uncertainty.
Research Insight:
Studies have shown that tailored exercise programs for heart failure patients improve cardiac output, reduce symptoms, and enhance quality of life — especially when strength and aerobic elements are combined under supervision. Even in moderate-to-severe HFrEF, regular activity can raise ejection fraction, boost stroke volume, and enhance muscle oxygen utilization (Taylor et al., Cochrane Review, 2019).
What “Training” Now Means
Training with HFrEF doesn't mean stopping — it means switching gears:
You won’t max out anymore, but you’ll still show up and put in work.
You won’t chase PRs, but you’ll chase progress that supports longevity.
You won’t always feel explosive, but you’ll build efficiency, strength, and metabolic resilience — in ways that are just as impressive.
It’s no longer about lifting the heaviest or running the fastest — it’s about strategic effort, intelligent recovery, and measured intensity that supports your heart, rather than stressing it.
This isn’t a downgrade. It’s a re-engineering of your athletic potential.
Redefining "Training Hard" Post-Diagnosis
When you’ve built your identity around performance, “training hard” isn’t just about effort — it’s a part of who you are. But after a heart failure diagnosis, especially HFrEF, the definition of “hard” has to shift. Not because you’ve become weak — but because the parameters have changed.
Hard now means:
Showing restraint when your ego tells you to push.
Listening to your body more than your stopwatch or training app.
Focusing on recovery as a performance tool, not a passive state.
Tracking cardiac function and symptom patterns with as much attention as you once gave your PRs.
Your intensity is still there. But now it’s tempered by intelligence, grounded in safety, and redefined around long-term capability. Think of it not as stepping back — but stepping sideways, onto a path where the goal is resilience over recklessness.
Prioritize Safety and Medical Guidance
Before resuming or overhauling your training, foundational medical input is essential. It’s not about getting permission to exercise — it’s about gathering the data you need to train effectively and safely.
Consult Your Cardiologist
Talk openly about your fitness history, goals, and what type of training you’d like to return to. Many cardiologists will encourage exercise, but few will assume you're aiming for hypertrophy blocks or 60-minute circuits unless you tell them. Set expectations early.
Undergo a Cardiac Stress Test
A stress test (with ECG monitoring) helps define your maximum tolerated heart rate, oxygen saturation during exertion, and symptom thresholds. It’s your new personalized ceiling — not a guess.
Ask your team:
“What heart rate range should I stay within?”
“What symptoms mean I should stop?”
“Is beta-blocker use changing my perceived effort?”
Consider Cardiac Rehabilitation
If offered, don’t skip cardiac rehab just because you’re “too advanced.” These programs help you ease into training while monitored — and you'll likely progress faster than average patients. More importantly, it creates a safe data record that builds trust with your medical team.
Adjust Training Intensity and Volume
The biggest mistake fit individuals make post-diagnosis is trying to train the way they always have — but slightly less. That approach is often still too much. Instead, rebuild your foundation from the ground up.
Monitor Intensity
Use the Borg Rating of Perceived Exertion (RPE) — not heart rate alone, especially if you're on meds like beta-blockers. Aim for an RPE of 12–14 (“somewhat hard”) for most cardio sessions. You should feel challenged, but not drained.
Modify Volume Strategically
Reduce overall training volume by:
Cutting total sets (e.g., 2 instead of 4)
Lowering time under tension (TUT)
Taking longer rest intervals (90–120 seconds between strength sets)
Don’t stack fatigue across days — spread intensity out, and allow more frequent low-effort sessions for movement quality and recovery.
Incorporate Purposeful Rest Days
This isn’t about being “lazy.” It's about giving your cardiac muscle time to adapt, not just your skeletal muscles. In HFrEF, overreaching can lead to decompensation, fatigue, or even hospitalization. Be consistent — not aggressive.
Embrace New Metrics of Progress
If your only yardstick is bench press max or split time, heart failure will feel like constant regression. But progress now looks different — and it’s just as valid.
Improved Ejection Fraction
Some patients experience a measurable increase in EF% through lifestyle and medical management — including exercise. Ask your doctor for periodic echocardiograms to track improvements.
Enhanced Quality of Life
Are you less winded doing daily tasks? Is your energy more stable? Are you sleeping better? These are functional gains that matter deeply.
Consistent Training Adherence
Being able to train three times a week for six months without crashing or symptom spikes? That’s performance. Consistency is now a cardiac achievement, not just a discipline flex.
Effective Training Strategies for Athletes with Heart Failure
With smart planning, you can still follow a structured training regimen. Here’s how to adjust the key elements without compromising your drive or identity.
Aerobic Exercise
Goal: Improve oxygen delivery and cardiac output without overstressing the system.
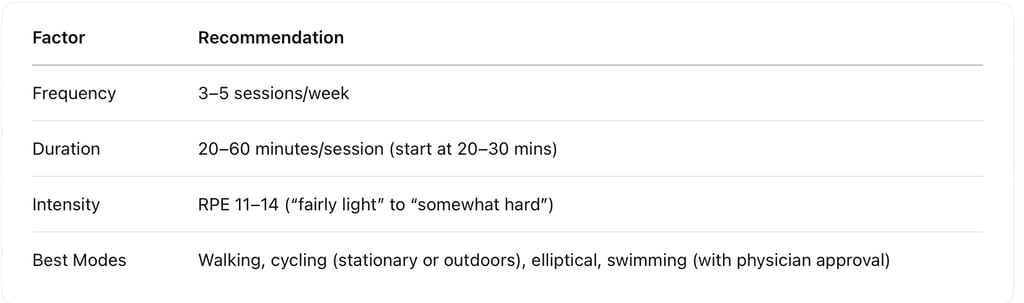
💡 Tip for Athletes: Use intervals — not max-intensity intervals, but structured pacing (e.g., 3 minutes brisk, 2 minutes easy) to add variation without spiking HR too far.
Resistance Training
Goal: Maintain strength, lean mass, and musculoskeletal function — while avoiding excessive load or intra-thoracic pressure.
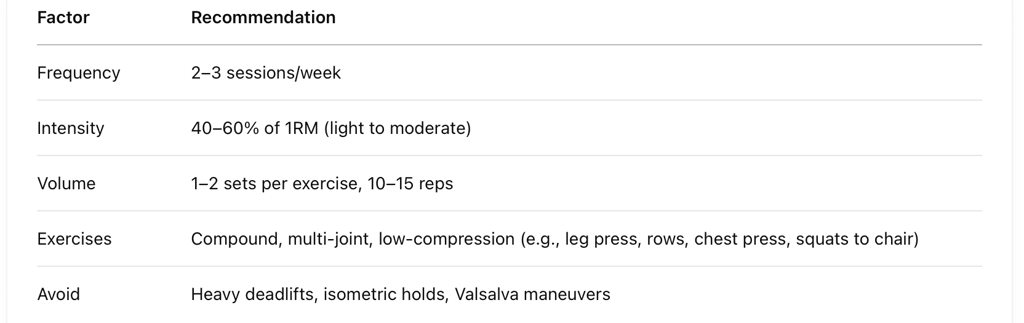
Tip: Use controlled tempos (2–1–2) to focus on quality, reduce blood pressure spikes, and get more from lighter loads.
Flexibility and Balance Work
Goal: Enhance joint mobility, reduce injury risk, support neuromuscular control — especially if you’ve lost confidence in your movement since diagnosis.
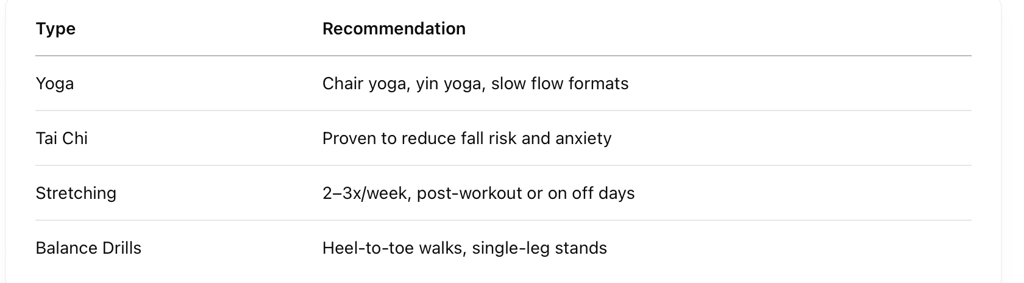
Mind-Body Benefit: These sessions can lower stress hormones, which directly affect heart rate variability and inflammation — making them valuable recovery tools, not just “filler.”
Psychological Adaptation and Motivation
For lifelong athletes, a heart failure diagnosis can be just as emotionally jarring as it is physically limiting. You’ve built an identity around pushing through limits, striving for performance, and embracing discomfort in the name of growth. Suddenly, your most trusted outlet—your body—is under new rules. That shift can feel like a betrayal.
But here’s what’s also true: your mental strength, your consistency, and your experience in overcoming plateaus are still with you. They’re not erased by diagnosis — they’re simply being redirected.
To adapt successfully, it’s not about lowering expectations. It’s about changing what success looks like, then building a mindset that allows you to pursue it fully.
Set Realistic, Purpose-Driven Goals
You’re still a goal-oriented person — that doesn’t change. What changes is how you define “progress.”
Instead of chasing PRs or aesthetics, redirect your goals toward metrics that preserve your health and athletic longevity:
Walk 3 miles without shortness of breath
Complete 3 strength sessions in a week with no cardiac symptoms
Improve ejection fraction or reduce resting heart rate over 6 months
Build consistency across months, not weeks
These aren’t consolation goals — they’re health performance goals, and they deserve as much celebration as a 405 lb squat ever did.
Engage with Support Networks
The isolation that can come with heart failure is real — especially for athletes, who often feel like they "should" be handling it on their own.
Consider:
Joining a heart failure or chronic illness community (in person or online)
Connecting with others who are active and managing the same diagnosis
Talking to a therapist or counselor experienced in identity loss, chronic disease, or sports psychology
There’s power in knowing you’re not alone. Shared stories often become shared strength.
Celebrate Small Victories — Because They’re Not Small
When you go from 5-day-a-week training to carefully managing your energy across a handful of sessions, even a single great workout is a win. So is waking up with more energy, completing a stretch of symptom-free weeks, or improving your mental state around the diagnosis.
Acknowledge:
Days when you feel strong
Weeks when you stay consistent
Moments when you rest because it’s smart, not because you “gave up”
This shift in focus is not about surrender — it’s about strategic evolution. You’re not giving up on being an athlete. You’re redefining what it means to be one under new, smarter terms.
Conclusion — Thriving in Your New Athletic Reality
A diagnosis of HFrEF may change your trajectory, but it doesn’t cancel your identity.
You’re still an athlete. You’re still someone who values effort, structure, and discipline. The only difference now is that your training has a higher purpose — not just performance, but protection. Not just growth, but longevity. Not just strength, but survival with strength.
With the right strategy, guidance, and mindset, you can:
Train consistently
Maintain muscle mass and cardiovascular health
Improve energy, stability, and even cardiac function
Stay empowered, informed, and in control of your body
This isn’t the end of your story — it’s a new chapter with higher stakes and deeper meaning.
“The weights are lighter. The pacing is slower. But the mission is greater. You’re still in the arena — you’re just playing smarter than ever.”
As always, consult with your cardiologist before starting or modifying your program, especially if you're considering resistance training, longer cardio sessions, or introducing new modalities. Get the green light — then get to work.
Reference List
European Society of Cardiology (ESC). (2020). 2020 ESC Guidelines on Sports Cardiology and Exercise in Patients with Cardiovascular Disease. European Heart Journal, 41(1), 1–78. European Society of Cardiology
Volterrani, M., et al. (2023). Effects of Concurrent, Within-Session, Aerobic and Resistance Exercise Training on Functional Capacity and Muscle Performance in Elderly Male Patients with Chronic Heart Failure. Journal of Clinical Medicine, 12(3), 750. MDPI
Pelliccia, A., et al. (2019). Recommendations for Participation in Competitive and Leisure Sport in Athletes with Cardiomyopathies, Myocarditis, and Pericarditis: Position Statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC). European Heart Journal, 40(1), 19–33. American College of Cardiology
Cleveland Clinic. (2023). Exercise and Activity for Patients with Heart Failure. Retrieved from
https://my.clevelandclinic.org/departments/heart/patient-education/recovery-care/heart-failure/exercise-activityAmerican Heart Association. (2022). Resistance Exercise Training in Individuals With and Without Cardiovascular Disease: 2022 Update. Circulation, 146(15), e1–e10. Ahá Journals
Wisløff, U., et al. (2007). Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation, 115(24), 3086–3094.
https://pubmed.ncbi.nlm.nih.gov/17548726/
